Abstract
Background: PCNSL is an Extranodal Non-Hodgkin Lymphoma (NHL), corresponding to 2.2% of all Central Nervous System (CNS) tumors and 1% of total NHL. It may develop in the brain, leptomeninges, spinal cord, or eyes, and is associated with a poor prognosis (median Overall Survival- OS: 30 months, when treated with High Dose Methotrexate based Therapy- HDMBT). There is scarce medical literature and further information is urgently needed to better categorize/evaluate this enthity.
Purpose: To evaluate the clinical outcome and the risk of death in patients with DLBCL PCNSL in a mixed ethnicity population (Brazil), to describe the characteristics of these patients.
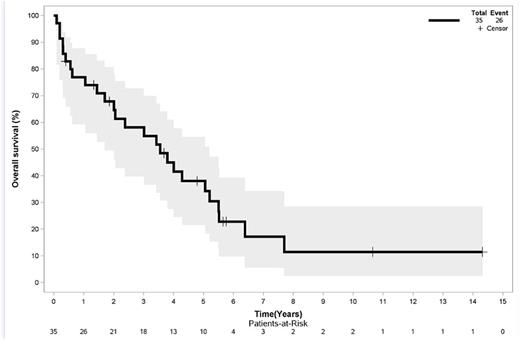
Methods: Retrospective observational study. Patients diagnosed with DLBCL PCNSL, HIV negative and not immunosuppressed were identified in the biggest academic Brazilian Cancer Institute- ICESP- from 1995 to 2016 (n=35). All histopathology slides and blocks were reviewed by a trained pathologist. OS and Progression Free Survival-PFS- were estimated using Kaplan-Meier analysis. Univariate Cox regression analysis was used to assess the association between clinical characteristics and the survival endpoints.
Results: Thirty-five patients with diagnosis of DLBCL PCNSL were identified between January 1995 and December 2016 at ICESP. Data was available for all 35 patients. Mean age at diagnosis: 66.7 years (SD: 15.88). Immunohistochemistry: CD20+: 94% (missing: 6%), high Ki67: 80% (missing: 20%), CD10+: 11.4% (missing: 57%), BCL6+: 17% (missing: 62%), MUM1+: 25% (missing: 65%). Cerebral Spinal Fluid (CSF) cytology was negative in 90.6%. Most patients had Performance Status PS 2-4 at diagnosis (66.7%), were male (54.3%), had involvement of Deep Brain Structures (79.4%). IELSG score: 0-1: 17%, 2-3: 45%, 4-5: 28%. Most patients received at least 1 line of treatment (94.3%), and most received HDMBT(80%). Twenty-six patients (74%) died (date of analysis: 01/06/2017). OS in 1, 5 and 10 years were 76.9 % (95% CI 56.1-87.7), 38.1% (95% CI 21-54.5) and 11.4 (95% CI 2.3-28.6), respectively. PFS in 1 and 5 years were 68.2% (95% CI 50-81) and 25.1% (95% CI 11.5-41.4), respectively. At Univariate Cox Regression, PS 2-4 compared to PS 0-1 at diagnosis was associated with increased risk of death (HR: 3.58, 95% CI: 1.29-9.91, p=0.014) and an increased risk of disease progression (HR: 2.61, 95% CI: 1.02-6.70, p=0.046).
Conclusions: This is the largest Brazilian cohort with PCNSL reported so far. PCNSL is an aggressive tumor with worse prognosis compared to systemic DLBCL. Despite the small series of patients to perform a risk factor analysis, poor Performance Status seems to be associated with decreased OS and PFS rates- as suggested by the MSKK Prognostic Model. Further biomarker analysis and clinical correlation are needed, and are under investigation for these patients, in order to identify better prognostic and predictive biomarkers.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal